What to Know About Myelodysplastic Syndrome and Its Treatments
Myelodysplastic syndrome (MDS) is a rare blood disorder affecting bone marrow function and healthy blood cell production. Learn how MDS is diagnosed, what treatments are available, and why early medical support and monitoring are key to managing symptoms and improving quality of life.
What is Myelodysplastic Syndrome?
Myelodysplastic Syndrome is a rare blood disorder that occurs when the bone marrow fails to produce enough healthy blood cells. In MDS, the immature blood cells (stem cells) in the bone marrow do not develop properly, leading to a decrease in one or more types of blood cells. This can result in anemia, increased risk of infections, and bleeding problems. MDS is often considered a type of blood cancer and can sometimes progress to acute myeloid leukemia (AML).
What are the causes of Myelodysplastic Syndrome?
The exact causes of Myelodysplastic Syndrome are not fully understood, but several factors have been identified as potential contributors:
-
Age: MDS is more common in older adults, with most cases diagnosed in people over 60 years old.
-
Previous cancer treatments: Chemotherapy and radiation therapy can increase the risk of developing MDS.
-
Exposure to certain chemicals: Long-term exposure to benzene and other industrial chemicals may raise the risk of MDS.
-
Genetic factors: Some inherited conditions, such as Fanconi anemia, can predispose individuals to MDS.
-
Environmental factors: Exposure to radiation or certain herbicides and pesticides may increase the risk.
It’s important to note that in many cases, the cause of MDS remains unknown, and these risk factors don’t necessarily lead to the development of the condition.
What are the symptoms of Myelodysplastic Syndrome?
Myelodysplastic Syndrome symptoms can vary widely among patients, and some may not experience any noticeable signs in the early stages. Common symptoms include:
-
Fatigue and weakness due to anemia (low red blood cell count)
-
Shortness of breath, especially during physical activities
-
Pale skin
-
Easy bruising or bleeding
-
Frequent infections or fevers
-
Petechiae (small red or purple spots on the skin)
-
Unexplained weight loss
These symptoms can be subtle and may develop gradually over time. If you experience persistent fatigue, frequent infections, or unusual bruising or bleeding, it’s essential to consult a healthcare professional for proper evaluation.
How is Myelodysplastic Syndrome diagnosed?
Diagnosing Myelodysplastic Syndrome typically involves a combination of tests and procedures:
-
Blood tests: Complete blood count (CBC) to check levels of red blood cells, white blood cells, and platelets.
-
Bone marrow biopsy and aspiration: A small sample of bone marrow is extracted and examined under a microscope to assess cell structure and composition.
-
Cytogenetic analysis: This test looks for chromosomal abnormalities in bone marrow cells.
-
Flow cytometry: A method used to analyze the characteristics of blood or bone marrow cells.
-
Molecular testing: This can help identify specific genetic mutations associated with MDS.
Once diagnosed, doctors use classification systems like the World Health Organization (WHO) classification or the International Prognostic Scoring System (IPSS) to determine the subtype and severity of MDS, which guides treatment decisions.
What treatments are available for Myelodysplastic Syndrome?
Treatment for Myelodysplastic Syndrome varies depending on the subtype, severity, and individual patient factors. The main goals of treatment are to manage symptoms, improve quality of life, and prevent progression to AML. Common treatment approaches include:
-
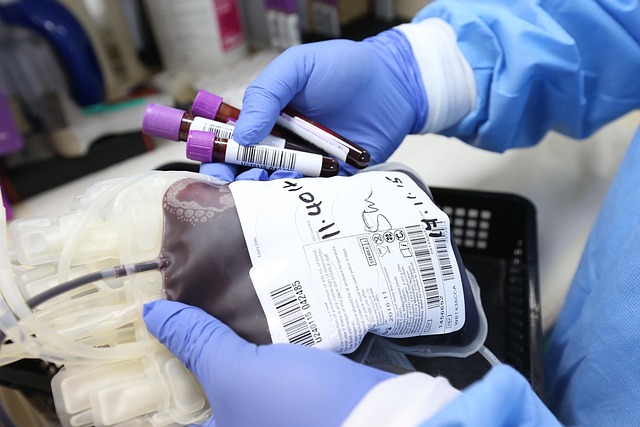
Supportive care: Blood transfusions, growth factors, and antibiotics to manage symptoms and complications.
-
Chemotherapy: Low-dose chemotherapy drugs like azacitidine or decitabine may be used to slow disease progression.
-
Immunosuppressive therapy: Drugs that suppress the immune system can be effective in some cases.
-
Lenalidomide: This drug is particularly effective for patients with a specific chromosomal abnormality (deletion 5q).
-
Stem cell transplantation: For eligible patients, this can be a potentially curative treatment option.
-
Clinical trials: Participation in research studies may provide access to new and innovative treatments.
Treatment decisions are made on a case-by-case basis, considering the patient’s overall health, preferences, and specific MDS characteristics.
How much does Myelodysplastic Syndrome treatment cost?
The cost of Myelodysplastic Syndrome treatment can vary significantly depending on the specific treatment approach, duration, and location. Here’s a general overview of potential costs:
| Treatment Type | Estimated Cost Range (USD) | Notes |
|---|---|---|
| Supportive Care | $1,000 - $5,000 per month | Includes blood transfusions and growth factors |
| Chemotherapy | $1,000 - $12,000 per cycle | Varies based on drug and administration method |
| Immunosuppressive Therapy | $2,000 - $10,000 per month | Depends on specific medications used |
| Lenalidomide | $10,000 - $15,000 per month | Cost may vary based on dosage |
| Stem Cell Transplantation | $350,000 - $800,000 total | Includes pre- and post-transplant care |
Prices, rates, or cost estimates mentioned in this article are based on the latest available information but may change over time. Independent research is advised before making financial decisions.
It’s important to note that these costs are often covered in part by health insurance, and various financial assistance programs may be available to help patients manage expenses. Patients should discuss costs and coverage options with their healthcare providers and insurance companies.
In conclusion, Myelodysplastic Syndrome is a complex blood disorder that requires careful management and ongoing medical support. While it can be a challenging diagnosis, advances in treatment options have improved outcomes for many patients. Early detection, proper diagnosis, and personalized treatment plans are key to managing MDS effectively and maintaining the best possible quality of life.
This article is for informational purposes only and should not be considered medical advice. Please consult a qualified healthcare professional for personalized guidance and treatment.




