Understanding Treatment Options for Tardive Dyskinesia
Tardive dyskinesia can affect movement and quality of life, but today’s treatment options offer practical relief. Explore how personalized therapies and professional care can help reduce symptoms, support daily function, and restore confidence over time.
What Are Current Treatments for Tardive Dyskinesia?
Medical professionals now have several evidence-based options for treating tardive dyskinesia. FDA-approved medications like deutetrabenazine and valbenazine specifically target the neurochemical imbalances that cause involuntary movements. These VMAT2 inhibitors work by regulating dopamine levels in the brain, effectively reducing the severity and frequency of abnormal muscle contractions. Additionally, healthcare providers may adjust or discontinue the original medications that triggered the condition, though this approach requires careful monitoring to avoid withdrawal complications or psychiatric symptom recurrence.
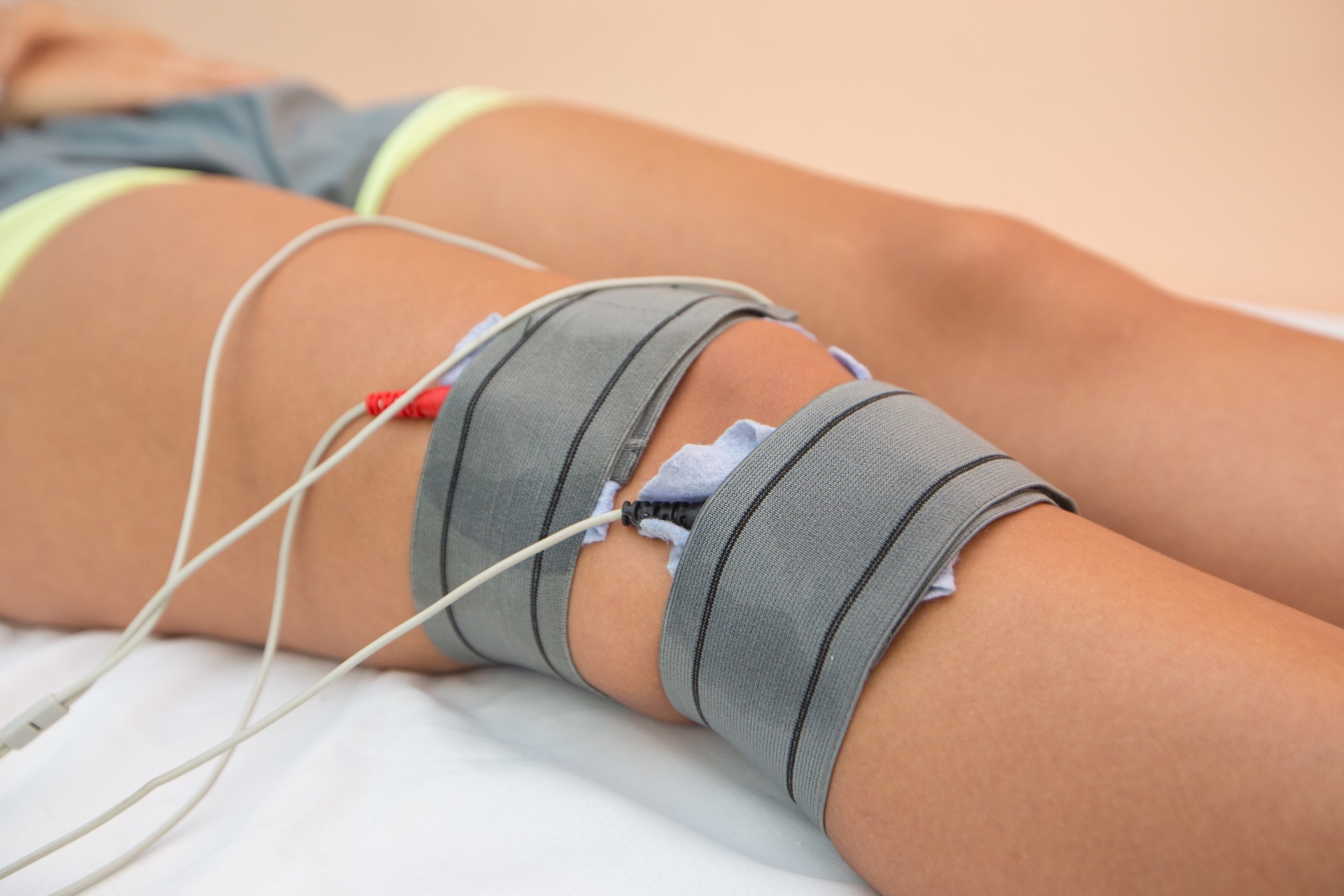
How Does Managing Involuntary Muscle Movements Work?
Managing involuntary muscle movements requires a multifaceted approach that combines medication management with lifestyle modifications. Physical therapy plays a crucial role in maintaining muscle strength and coordination while teaching patients adaptive techniques for daily activities. Occupational therapists help individuals develop strategies for eating, writing, and performing work-related tasks despite movement challenges. Speech therapy becomes essential when tardive dyskinesia affects facial muscles and tongue movement, impacting communication and swallowing safety. Regular monitoring through standardized assessment scales allows healthcare teams to track progress and adjust treatment intensity accordingly.
Why Is Combining Therapy and Medical Care Essential?
The integration of therapeutic interventions with medical treatment creates synergistic effects that neither approach can achieve alone. While medications address the underlying neurochemical causes, therapeutic interventions help patients develop coping mechanisms and maintain functional independence. Counseling support addresses the psychological impact of living with a visible movement disorder, helping patients manage anxiety, depression, and social concerns that often accompany tardive dyskinesia. This comprehensive approach recognizes that effective treatment must address both the physical symptoms and the emotional well-being of patients and their families.
What Long-Term Approaches to Symptom Control Exist?
Successful long-term management focuses on preventing symptom progression while maximizing current function. Regular medication reviews ensure optimal dosing and minimize side effects, while periodic assessments using standardized rating scales track changes over time. Some patients benefit from botulinum toxin injections for localized muscle groups, particularly when facial or neck movements are prominent. Deep brain stimulation represents an emerging option for severe cases that don’t respond to conventional treatments, though this approach requires careful patient selection and specialized medical centers.
How Can Treatment Support Improving Daily Function?
In the United States, comprehensive tardive dyskinesia care often involves specialized movement disorder centers that bring together neurologists, psychiatrists, and rehabilitation specialists under one roof. The Michael J. Fox Foundation and similar organizations have funded research initiatives that have led to breakthrough treatments becoming available at major medical centers like Mayo Clinic, Cleveland Clinic, and Johns Hopkins. Many patients find success through telemedicine consultations, which have become increasingly accessible since 2020, allowing rural communities to access specialist care without extensive travel. Support groups, both in-person and virtual, provide valuable peer connections and practical tips for managing daily challenges.
What Treatment Options and Costs Should Patients Consider?
Treatment costs vary significantly depending on insurance coverage, geographic location, and specific interventions required. Specialist consultations typically range from $300 to $800 per visit, while FDA-approved medications can cost $3,000 to $8,000 monthly without insurance coverage. Physical therapy sessions average $75 to $150 per session, with most patients requiring 8-12 sessions initially.
| Treatment Type | Provider Examples | Monthly Cost Range |
|---|---|---|
| Specialist Consultation | Mayo Clinic, Cleveland Clinic | $300-$800 per visit |
| FDA-Approved Medications | Teva (Austedo), Neurocrine (Ingrezza) | $3,000-$8,000 |
| Physical Therapy | Local rehabilitation centers | $600-$1,800 |
| Counseling Support | Licensed therapists | $400-$800 |
Prices, rates, or cost estimates mentioned in this article are based on the latest available information but may change over time. Independent research is advised before making financial decisions.
Most insurance plans, including Medicare, provide coverage for FDA-approved tardive dyskinesia medications, though prior authorization requirements are common. Patient assistance programs from pharmaceutical manufacturers can significantly reduce out-of-pocket costs for qualified individuals. Many treatment centers offer payment plans or sliding scale fees for therapy services.
The landscape of tardive dyskinesia treatment continues evolving as researchers develop new therapeutic targets and refine existing approaches. Early intervention remains crucial for optimal outcomes, emphasizing the importance of recognizing symptoms promptly and seeking specialized care. With proper medical management and comprehensive support services, many patients experience significant improvement in their symptoms and overall quality of life, allowing them to maintain independence and pursue meaningful activities.
This article is for informational purposes only and should not be considered medical advice. Please consult a qualified healthcare professional for personalized guidance and treatment.




