Hemoglobinuria: Unexpected Signals You Must Not Ignore
Hemoglobinuria is a rare but serious condition that may silently signal underlying health issues. While often unnoticed in early stages, certain unexpected symptoms could point to a more significant problem. Understanding these signs is essential for timely diagnosis and treatment. This article uncovers the key warning signals of hemoglobinuria and what they could mean for your health.
What Are Early Signs of Hemoglobinuria You Might Overlook?
The early indicators of hemoglobinuria frequently present as subtle changes that patients and even healthcare providers might initially dismiss. Dark-colored urine, particularly noticeable in the morning, serves as the most recognizable symptom. However, many individuals overlook other critical signs including unexplained fatigue, shortness of breath during routine activities, and frequent headaches.
Abdominal pain, particularly in the upper regions, often accompanies hemoglobinuria but gets attributed to digestive issues. Patients may also experience difficulty swallowing, erectile dysfunction in men, and an increased tendency toward blood clots. These symptoms develop gradually, making them easy to rationalize as stress-related or age-related changes rather than indicators of a serious underlying condition.
Sleep disturbances and cognitive difficulties, including problems with concentration and memory, also characterize early hemoglobinuria. Many patients report feeling mentally foggy or experiencing mood changes that seem unrelated to their physical symptoms, creating a complex clinical picture that requires careful evaluation.
How Hemoglobinuria Could Indicate a Deeper Health Issue?
Hemoglobinuria serves as a warning signal for several serious underlying conditions that require immediate medical intervention. Paroxysmal nocturnal hemoglobinuria represents an acquired genetic disorder affecting blood cell membranes, making them vulnerable to destruction by the body’s complement system. This condition can lead to life-threatening complications including thrombosis, kidney damage, and bone marrow failure.
The presence of hemoglobin in urine may also indicate autoimmune hemolytic anemia, where the immune system mistakenly attacks healthy red blood cells. Additionally, certain infections, particularly malaria, can trigger massive red blood cell destruction leading to hemoglobinuria. Mechanical causes, such as artificial heart valves or intense physical exercise, can also result in red blood cell breakdown.
More concerning, hemoglobinuria sometimes signals underlying malignancies affecting blood cell production or function. Certain medications, including some antibiotics and anti-inflammatory drugs, can trigger hemolytic episodes in susceptible individuals. Understanding these connections emphasizes why hemoglobinuria requires comprehensive medical evaluation rather than symptomatic treatment alone.
Important Diagnostic Steps for Detecting Hemoglobinuria Early
Accurate diagnosis of hemoglobinuria requires a systematic approach combining clinical assessment with specialized laboratory testing. Initial evaluation begins with a comprehensive medical history focusing on symptom patterns, medication use, and family history of blood disorders. Physical examination should assess for signs of anemia, jaundice, and organ enlargement.
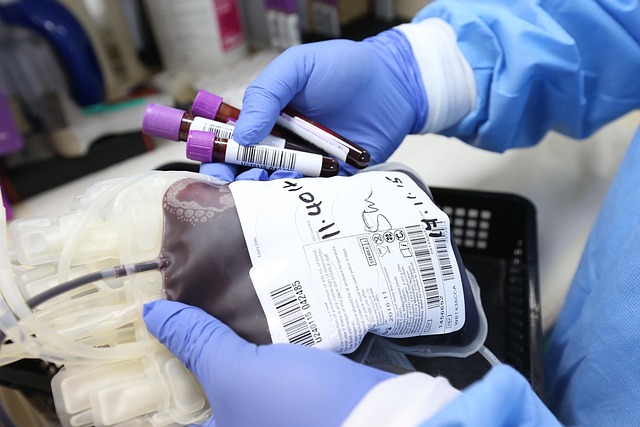
Laboratory testing forms the cornerstone of hemoglobinuria diagnosis. Urinalysis reveals the presence of hemoglobin without intact red blood cells, distinguishing hemoglobinuria from hematuria. Complete blood count with peripheral blood smear helps identify specific blood cell abnormalities and signs of hemolysis. Lactate dehydrogenase levels typically elevate during hemolytic episodes, while haptoglobin levels decrease as this protein binds free hemoglobin.
Flow cytometry testing proves essential for diagnosing paroxysmal nocturnal hemoglobinuria by detecting the absence of specific surface proteins on blood cells. Additional tests may include direct and indirect Coombs tests to identify autoimmune causes, and specialized genetic testing when hereditary conditions are suspected. Regular monitoring through repeat testing helps track disease progression and treatment response.
Myths About Hemoglobin in Urine and How to Approach Them
Several misconceptions surrounding hemoglobinuria can delay proper diagnosis and treatment. One persistent myth suggests that dark urine always indicates dehydration or dietary factors, leading patients to increase fluid intake without seeking medical evaluation. While hydration affects urine concentration, true hemoglobinuria requires medical intervention regardless of fluid status.
Another common misconception involves the belief that hemoglobinuria only affects elderly individuals or those with obvious blood disorders. In reality, paroxysmal nocturnal hemoglobinuria can develop at any age, with many cases diagnosed in young adults. The intermittent nature of symptoms often reinforces the myth that occasional dark urine isn’t serious, when in fact episodic hemoglobinuria may indicate PNH.
Some patients believe that hemoglobinuria will resolve spontaneously without treatment. This dangerous assumption can lead to severe complications including kidney damage, stroke, or pulmonary embolism. Modern treatment approaches, including complement inhibitor therapies, can effectively manage hemoglobinuria when initiated promptly. Healthcare providers must address these myths directly while educating patients about the importance of ongoing medical supervision and treatment compliance.
Effective management of nocturnal hemoglobinuria has evolved significantly with the introduction of targeted therapies. Treatment typically involves complement system inhibitors, supportive care for anemia, and anticoagulation therapy to prevent thrombotic complications. The comprehensive approach requires regular monitoring and adjustment based on individual patient response and disease progression.
Conclusion
Recognizing hemoglobinuria early can prevent serious complications and improve long-term outcomes for affected individuals. The combination of subtle early symptoms, potential for severe underlying conditions, and availability of effective treatments makes awareness and prompt medical evaluation crucial. By understanding the warning signs, diagnostic processes, and dispelling common myths, patients and healthcare providers can work together to ensure timely intervention. Anyone experiencing persistent dark urine or related symptoms should seek immediate medical consultation for proper evaluation and potential treatment.
This article is for informational purposes only and should not be considered medical advice. Please consult a qualified healthcare professional for personalized guidance and treatment.




