Crohn’s Disease in Seniors: Warning Signs You Shouldn’t Miss
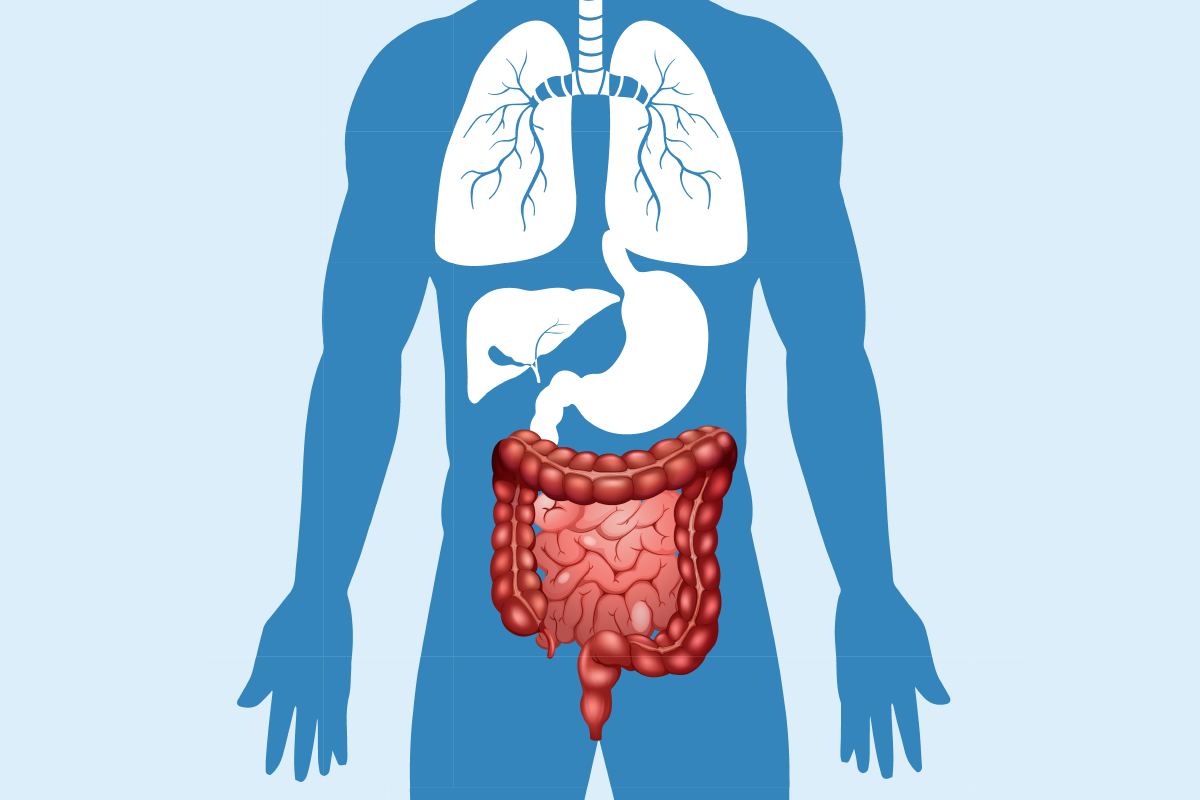
Crohn’s disease can affect people at any age, but when it appears later in life, symptoms may be overlooked or mistaken for other digestive issues. In seniors, fatigue, weight loss, abdominal pain, or unusual bowel habits can be early red flags. This guide explains how Crohn’s disease presents in older adults, why timely diagnosis matters, and what to watch for before it worsens.
What Are Crohn’s Symptoms in Older Adults?
Crohn’s disease symptoms in seniors can be subtle and develop gradually, making them easy to dismiss as normal aging. The most common signs include persistent diarrhea lasting more than a few weeks, often accompanied by blood or mucus. Abdominal cramping and pain, particularly in the lower right area, may come and go initially but can become more frequent over time.
Unexplained weight loss is another significant indicator, especially when combined with decreased appetite. Many seniors also experience chronic fatigue that doesn’t improve with rest, along with low-grade fever that persists without an obvious cause. Joint pain and stiffness may also accompany digestive symptoms, as Crohn’s disease can affect areas beyond the intestinal tract.
Additional symptoms include mouth sores, skin irritations, and eye inflammation. These seemingly unrelated issues often occur because Crohn’s disease is an autoimmune condition that can impact multiple body systems simultaneously.
How Does Crohn’s Differ in Seniors vs Younger Adults?
The presentation of Crohn’s disease varies significantly between age groups, with seniors often experiencing milder initial symptoms that progress more slowly. Unlike younger patients who typically develop symptoms in their twenties or thirties, seniors may not experience the severe abdominal pain and dramatic weight loss that characterizes early-onset disease.
In older adults, Crohn’s disease more commonly affects the colon rather than the small intestine, leading to different symptom patterns. Seniors are also more likely to experience complications such as strictures or blockages earlier in the disease course, partly due to age-related changes in tissue healing and immune function.
Another key difference lies in diagnosis timing. Younger adults often receive faster diagnoses because their symptoms are more dramatic and occur in otherwise healthy individuals. Seniors, however, may have multiple health conditions that mask or mimic Crohn’s symptoms, leading to delayed recognition and treatment.
The response to treatment can also vary, as older adults may have slower healing rates and increased sensitivity to certain medications used to manage Crohn’s disease.
What Digestive Warning Signs Shouldn’t Be Ignored After 60?
Several digestive symptoms warrant immediate medical attention in adults over 60, as they may indicate Crohn’s disease or other serious conditions. Persistent changes in bowel habits, including new-onset diarrhea lasting more than two weeks or alternating constipation and diarrhea, should never be dismissed as normal aging.
Blood in stool, whether bright red or dark and tarry, requires urgent evaluation. Even small amounts of blood that appear intermittently can signal inflammation in the digestive tract. Similarly, severe abdominal pain that interferes with daily activities or sleep patterns needs professional assessment.
Unintentional weight loss of more than five pounds over a few months, particularly when accompanied by reduced appetite, can indicate underlying inflammatory bowel disease. Night sweats, persistent low-grade fever, or feeling generally unwell without an obvious cause are additional red flags.
Changes in stool consistency, frequency, or appearance that persist beyond a few weeks should also prompt medical consultation. This includes unusually loose stools, increased urgency, or difficulty controlling bowel movements.
Early Detection Tips for Crohn’s in Seniors
Early detection of Crohn’s disease in seniors requires careful attention to subtle changes and proactive communication with healthcare providers. Keep a detailed symptom diary documenting bowel habits, pain levels, energy levels, and any other concerning symptoms for at least two weeks before medical appointments.
Regular health screenings become increasingly important after age 60, including routine blood tests that can detect anemia, inflammation markers, or nutritional deficiencies associated with Crohn’s disease. Don’t hesitate to request additional testing if symptoms persist despite normal initial results.
Family history plays a crucial role in early detection, so inform healthcare providers about any relatives with inflammatory bowel disease, even distant relatives. Genetic factors can increase susceptibility to Crohn’s disease at any age.
Maintaining open communication with primary care physicians about digestive symptoms, even those that seem minor, can lead to earlier referrals to gastroenterologists when necessary. Many seniors minimize symptoms or attribute them to aging, potentially delaying crucial treatment.
When Should You Talk to a Doctor About Bowel Changes?
Knowing when to seek medical attention for bowel changes can significantly impact treatment outcomes and quality of life. Schedule an appointment within a week if you experience persistent diarrhea lasting more than five days, especially with accompanying fever, severe cramping, or blood in stool.
Immediate medical attention is necessary for symptoms such as severe dehydration, high fever above 101°F, severe abdominal pain that prevents normal activities, or signs of intestinal obstruction including vomiting, inability to pass gas, and severe bloating.
For less urgent symptoms, such as gradual changes in bowel habits, mild cramping, or occasional loose stools, schedule an appointment within two to three weeks. Don’t wait for symptoms to worsen or resolve on their own, as early intervention often leads to better outcomes.
Additionally, discuss any new digestive symptoms during regular check-ups, even if they seem minor. Healthcare providers can determine whether symptoms warrant further investigation or monitoring. Remember that effective Crohn’s disease treatment depends heavily on early diagnosis and appropriate medical management.
This article is for informational purposes only and should not be considered medical advice. Please consult a qualified healthcare professional for personalized guidance and treatment.




